Melanoma: identified the micro-molecules produced by tumors to resist the therapies
The scientific collaboration between the National Cancer Institute Regina Elena (IRE), La Sapienza and the IRCCS Pascale of Naples, supported by the AIRC - Italian Association for Cancer Research, has produced interesting results on the treatment of melanoma. The researchers, coordinated by Gennaro Ciliberti of the National Cancer Institute Regina Elena and by Rita Mancini of the Department of Clinical and Molecular Medicine, investigated the role of microRNAs in resistance to therapies, opening new paths to the treatment of cancer. The results of the study are published in the journal Cell Death & Differentiation.
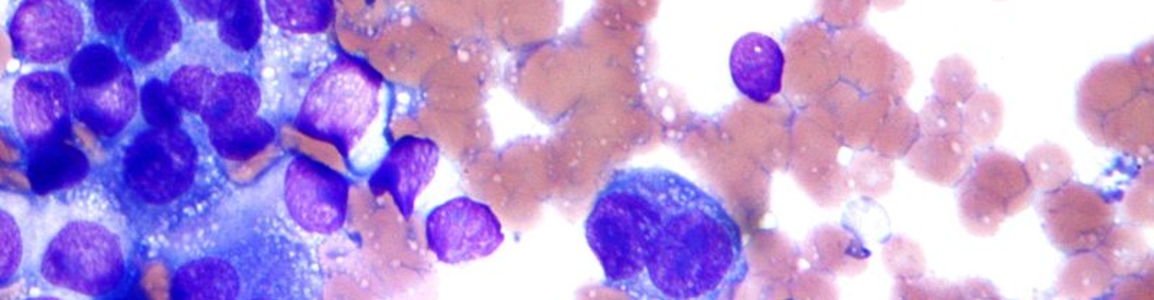
Through molecular biology techniques, the team observed that many microRNAs are present differently after the development of resistance to anti-BRAF drugs (the gene that gives rise to cancer, when mutated). Some are more present in resistant cells while others are less so. The hypothesis that originates from this observation is that melanoma to become resistant must evolve, getting rid of certain miRNAs and enriching itself with others.
Furthermore, it has been observed that if microRNAs are returned to normal levels in resistant melanoma cells, cells reacquire sensitivity to drugs. Another interesting feature of microRNAs produced by tumors is that they can be traced in human blood as liquid biopsy biomarkers (a test to diagnose tumors) in a simple and economical way. In particular, the working group has shown that some of the microRNAs studied are detectable in the blood of patients with melanoma and are able to indicate the development of resistance to therapy.
Melanoma is the most aggressive skin cancer and its incidence is gradually increasing, in large part due to the increased or more concentrated exposure to UV rays. About 7,300 new cases are estimated in Italy each year among men and 6,700 among women. The incidence is growing and as confirmed by the data of the Italian association of cancer registries (AIRTUM 2017), it has doubled over the last 10 years.
Until a few years ago, the metastatic form was considered a disease difficult to cure, but fortunately in recent years there have been important successes in the fight against this type of cancer. Current melanoma therapies are nowadays of two main types: immunotherapy with immunological checkpoint inhibitor antibodies and molecular, and target therapies with kinase inhibitor drugs (enzymes that affect the level of activity and function of proteins).
The development of the latter therapy starts from the discovery that in many cases this tumor is caused by the oncogene BRAF (an oncogene is a gene that, if mutated, gives rise to cancer). The altered protein produced by BRAF can be effectively affected with targeted therapies, capable of killing only the diseased cells, saving healthy ones. However, an obstacle still to be overcome is the development of resistance to treatments, a condition in which the response to therapy is partial or completely absent. Resistance can also occur during treatment, rendering previously used drugs useless and often leading to patient death.
From this fundamental clinical problem arise essential questions: if we can identify new molecules and drugs able to improve current care and, if and how it is possible to predict id a patient responds to therapies.
It is in this context that the new study is inserted, offering therapeutic and diagnostic opportunities that can be used to exert an increasing control of this disease if further deepened.
References:
Reprogramming miRNAs global expression orchestrates development of drug resistance in BRAF mutated melanoma - Luigi Fattore, Ciro Francesco Ruggiero, Maria Elena Pisanu, Domenico Liguoro, Andrea Cerri, Susan Costantini, Francesca Capone, Mario Acunzo, Giulia Romano, Giovanni Nigita, Domenico Mallardo, Concetta Ragone, Maria Vincenza Carriero, Alfredo Budillon, Gerardo Botti, Paolo Antonio Ascierto, Rita Mancini & Gennaro Ciliberto - Cell Death & Differentiation 2018 Sep, doi: 10.1038/s41418-018-0205-5.