A New Therapeutic Strategy for Cancer
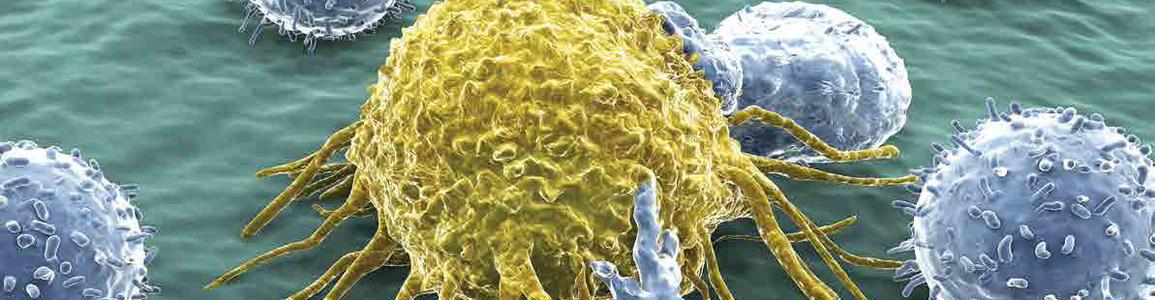
Cancer cells are crafty at evading the immune system. In fact, numerous studies have highlighted the ability of tumors to tamper with body’s immune responses by producing proteins like PD-L1, which brakes immune cells such as T lymphocytes.
In this context, the research coordinated by Sapienza Professor Pankaj Trivedi, in collaboration with Frank Slack’s group at Beth Israel Deaconess Medical Center of Harvard Medical School, suggests a new therapeutic approach for tumors of infectious origin. The results of the researchers suggest the potential of two combined actions may be applied to neutralize immuno-evasion mechanism: On the one hand, using antibodies which remove the brakes on T cells; on the other, by introducing small RNA molecules into the tumor cell so that it no longer produces the “braking” protein. The results of the study are published in the journal Leukemia.
Considering that about 15 % of all human tumors have an infectious origin, the research team identified the virus immune evasion mechanism put into action by Epstein-Barr virus (EBV). This virus is frequently associated with several human tumors like Burkitt lymphoma, diffuse large B cell lymphoma, Hodgkin lymphoma and nasopharyngeal carcinoma.
The interaction between the T cells and tumor cells and tumor immunogenicity were evaluated by 3D microfluidic chips, an innovative method developed by Eleni Anastasiadou, a graduate of Sapienza, currently at Harvard and first author of the study. Eleni Anastasiadou together with Slack and Trivedi have jointly patented their innovation of the RNA aided combinatorial immunotherapy. Using this method, the researchers studied molecular mechanisms and how the virus blocks immune responses. Several very aggressive tumors- explains Professor Trivedi- express PD-L1 on their cell surface, which by binding to PD-1 on T cells, deactivates them, thus deceiving our immune system”.
This study extends the cancer immunotherapy scenario, which today is mainly based on the use of monoclonal antibodies with a margin of success in only about 20-40% of cases. “The hope is that the combination of antibodies directed against PD-L1 and RNA molecules- concludes Professor Trivedi- may turn out to be more effective than traditional therapies”.
References:
Epstein−Barr Virus-encoded EBNA2 Alters Immune Checkpoint PD-L1 Expression by Downregulating miR-34a in B-cell Lymphomas - Eleni Anastasiadou, Dina Stroopinsky, Stella Alimperti, Alan L Jiao, Athalia R Pyzer, Claudia Cippitelli, Giuseppina Pepe, Martina Severa, Jacalyn Rosenblatt, Marilena P Etna, Simone Rieger, Bettina Kempkes, Eliana M Coccia, Shannan J Ho Sui, Christopher S Chen, Stefania Uccini, David Avigan, Alberto Faggioni, Pankaj Trivedi & Frank J Slack - Leukemia Published: 26 June 2018 DOI: 10.1038/s41375-018-0178-x
For further information
Pankaj Trivedi, Department of Experimental Medicine, Sapienza University
pankaj.trivedi@uniroma1.it (link sends e-mail)